Internal hemorrhoid removal surgery is a medical procedure to treat internal hemorrhoids that have become enlarged, swollen, and painful.
Internal hemorrhoids commonly affect millions worldwide and can cause discomfort, irritation, and bleeding.
This type of hemorrhoid occurs within the rectal canal and may not always be visible.
If left untreated, internal hemorrhoids can lead to complications such as blood clots, anal fissures, or even strangulation.
Internal hemorrhoids can be effectively removed with a minimally invasive procedure performed as an outpatient procedure.
Internal Hemorrhoid Removal Surgery:

Internal Hemorrhoid Removal Surgery is a medical procedure that is used to treat patients with internal hemorrhoids. This common condition affects many people and can cause discomfort and pain.
The surgery involves the removal of the hemorrhoids from the rectum and anus. During this procedure, the patient will be under general anesthesia, and a small incision will be made in the anus to access the hemorrhoids.
Rubber Band Ligation

The rubber band ligation procedure can help those with internal hemorrhoids. By placing a small rubber band around the base of the hemorrhoid, the blood supply to that area is cut off.
Over a few days, the hemorrhoid will wither away and fall off without any noticeable pain or discomfort. It's no wonder that many physicians prefer this treatment due to its low risks and impressive success rate.
Patients can return home the same day after rubber band ligation since it is typically performed, outpatient. It is usually done under local anesthesia, which numbs the area and ensures that the patient remains comfortable throughout the procedure. The only discomfort the patient may feel is a slight tingling or pressure while applying the rubber band.
The procedure is very safe and rarely causes any complications. However, in some cases, patients may experience bleeding, infection, or the formation of a blood clot around the treated area. These complications are rare and usually easily managed with a follow-up visit to the physician.
Rubber band ligation is a very effective and low-risk option for removing internal hemorrhoids. It has been proven to be a simple and effective treatment with a high success rate.
The best way to treat hemorrhoids is to seek medical attention from a trusted healthcare professional. Rubber band ligation is an effective internal hemorrhoid removal surgery.
Hemorrhoidectomy

Hemorrhoidectomy is a surgical procedure that is performed as a treatment for internal hemorrhoids. This type of surgery is considered the most effective and permanent solution to remove internal hemorrhoids. Swollen veins inside the anal canal can cause significant pain, discomfort, and bleeding.
During a Hemorrhoidectomy, the surgeon removes the inflamed tissue and the veins causing the problem. The surgical process may be performed under general, regional, or local anesthesia, depending on the procedure's complexity and the patient's medical history.
The surgeon may make an incision in the anal canal to effectively remove the hemorrhoids or use other methods, such as stapling, laser or infrared coagulation, or rubber band ligation.
Patients who undergo Hemorrhoidectomy are advised to take a period of rest to allow for proper healing to occur. In some cases, pain medication and stool softeners are prescribed to help alleviate pain and prevent constipation.
Follow the post-surgical instructions carefully to prevent disrupting the healing process, such as maintaining appropriate hygiene, lifting heavy objects, and not exercising.
As with any surgical procedure, Hemorrhoidectomy carries risks, such as bleeding, infection, and prolonged healing time. However, with proper consultation with certified and experienced surgeons, the risks can be minimized, and the recovery process can be successful.

Stapled Hemorrhoidopexy
Internal hemorrhoids are treated with stapled hemorrhoidopexy, or PPH (Procedure for Prolapse and Hemorrhoids).
During the procedure, a circular stapler removes a portion of the lining of the anal canal above the hemorrhoidal tissue, causing the hemorrhoids to shrink and be pulled back up into the anal canal. This stapling method results in less pain and bleeding than traditional hemorrhoidectomy surgery.
Stapled hemorrhoidopexy is recommended for those with prolapsed hemorrhoids, meaning they protrude outside the anus. Patients can go home the same day after the procedure since it is outpatient.
Recovery time is also reduced, most patients returning to normal activities within a week. However, as with any surgical procedure, there are potential risks associated with stapled hemorrhoidopexy.
These risks include bleeding, infection, and difficulty passing stool. Talking with a doctor about the best treatment option for individual circumstances and assessing this procedure's potential benefits and risks is essential.
Sclerotherapy

Internal hemorrhoids can cause discomfort, pain, and bleeding. Fortunately, a safe and effective surgical technique can help sclerotherapy.
Sclerotherapy involves injecting a unique solution into the hemorrhoid, causing it to shrink and eventually disappear. There is little downtime associated with this minimally invasive outpatient procedure.
Compared to other surgical techniques, sclerotherapy is less painful and has a lower risk of complications. Plus, it only takes a few minutes to complete.
If you suffer from internal hemorrhoids, talk to your healthcare provider to see if sclerotherapy suits you. Say goodbye to discomfort and pain with this quick and easy solution.
Coagulation Therapy

Coagulation is a popular internal hemorrhoid removal surgery used to stop bleeding from hemorrhoids by coagulating the blood vessels that supply them.
The procedure involves using an infrared coagulator or an electric probe that generates heat and is directed onto the internal hemorrhoids. This causes the blood vessels to seal off, which stops the bleeding and causes hemorrhoids to shrink over time.
Hemorrhoidectomy is an anesthesia- and incision-intensive procedure. Coagulation therapy, on the other hand, is minimally invasive. The procedure is performed in the doctor's office or clinic under topical anesthesia, usually taking less than 30 minutes to complete.
Coagulation therapy is a safe and effective procedure with a high success rate, with most patients experiencing complete relief from hemorrhoid symptoms after a single treatment. It has fewer complications and side effects than other surgical procedures, and patients can return to normal activities immediately after the procedure.
Coagulation therapy may not work for all types of hemorrhoids and advanced cases. It may also cause mild discomfort or pain during and after the procedure, but it typically disappears within a few days.

Electrocoagulation
Electrocoagulation is an innovative and effective surgical procedure used for internal hemorrhoid removal. An electric current prevents hemorrhoidal tissue from growing by searing it.
Electrocoagulation is a minimally invasive procedure that can be performed as an outpatient surgery. It is ideal for individuals who wish to avoid the discomfort and complications associated with traditional hemorrhoid removal surgeries.
During electrocoagulation, a device delivers an electric current to the hemorrhoidal tissues. This generates heat, causing blood vessels to be destroyed. As a result, the hemorrhoids shrink and fall off due to a lack of blood supply.
An electrocoagulation procedure can remove internal hemorrhoids quickly and effectively. After the surgery, patients only need a short recovery time, usually just a few days, before they can resume their normal daily activities.
Choose electrocoagulation to eliminate internal hemorrhoids today, and enjoy a fast and pain-free recovery!
Furthermore, electrocoagulation is preferred for internal hemorrhoid removal because it is less invasive than other surgical procedures, such as hemorrhoidectomy. Electrocoagulation is also less painful than traditional hemorrhoid removal surgeries, such as rubber band ligation, which require multiple treatments and can cause severe discomfort.
Hemorrhoidal Artery Ligation
Hemorrhoidal artery ligation, also known as Transanal Hemorrhoidal Dearterialization, is a minimally invasive surgical technique used to treat internal hemorrhoids. As a result, less blood flows to the hemorrhoidal cushions, and the internal hemorrhoids shrink.
A special anoscope is inserted into the rectum to locate the hemorrhoids during the procedure. A Doppler ultrasound probe is used to identify the hemorrhoidal arteries, which are then tied off with a suture.
This safe and effective treatment is performed under anesthesia and is typically associated with little to no discomfort.
Compared to invasive surgical procedures, such as hemorrhoidectomy, hemorrhoidal artery ligation has a high success rate with minimal complications. Patients can resume normal activities within a few days after the procedure and experience less pain, bleeding, and shorter recovery time.
Bipolar, Laser, or Infrared Coagulation

Internal hemorrhoids can cause pain, discomfort, and bleeding. While some cases can be treated with medications, lifestyle changes, or home remedies, others may require surgery.
Bipolar, laser, and infrared coagulation are three minimally invasive techniques commonly used for internal hemorrhoid removal surgery.
Bipolar coagulation involves using a particular device called a bipolar probe to apply energy to the hemorrhoidal tissue. This energy causes the tissue to thicken and shrink, eventually wholly removing it.
The procedure is usually performed under local anesthesia, and patients can generally return to their normal activities within a few days.
As the name suggests, laser coagulation uses a laser beam to destroy the hemorrhoidal tissue. The tissue absorbs the laser energy, causing it to vaporize and shrink.
This results in a much smaller and less painful hemorrhoid. Laser coagulation can be performed in an outpatient setting with local anesthesia, and the recovery time is relatively short.
Infrared Coagulation uses a light beam to coagulate the blood vessels carrying hemorrhoidal fluid. The heat from the light causes the vessels to shrink, reducing the size of the hemorrhoids.
This procedure is typically performed in a doctor's office and does not require anesthesia. Patients can resume their normal activities almost immediately after the procedure.
Conventional Hemorrhoidectomy

Conventional Hemorrhoidectomy is an internal hemorrhoid removal surgery involving the physical removal of hemorrhoids using traditional surgical techniques. During this procedure, the surgeon creates incisions around the swollen veins of the hemorrhoids and removes them completely.
Conventional hemorrhoidectomy may be recommended for patients who have large or symptomatic internal hemorrhoids that have not responded to other treatments. General anesthesia is used during this surgery, meaning the patient is asleep the entire time.
One of the primary benefits of conventional hemorrhoidectomy is that it is highly effective in treating severe internal hemorrhoids. Unlike other treatments, such as rubber band ligation or sclerotherapy, which are only effective in treating mild to moderate cases, conventional hemorrhoidectomy can successfully remove even the most stubborn hemorrhoids.
However, conventional hemorrhoidectomy is not without risks. Potential complications of this procedure may include bleeding, infection, and pain during bowel movements. Additionally, the recovery period after conventional hemorrhoidectomy can be several weeks, during which time patients may experience discomfort and require pain medication.
A conventional hemorrhoidectomy is a highly effective but invasive internal hemorrhoid removal surgery that is typically used for severe cases. While it is associated with a high success rate, it is important to discuss this procedure's potential risks and benefits with a medical professional to determine if it is the right choice for individual patients.
Doppler-Guided Transanal Hemorrhoidal Artery Ligation:

Transanal hemorrhoidal artery ligation (THD) can be used to remove hemorrhoids. This advanced surgical technique is gaining popularity as it is less painful, has fewer complications, and patients experience a faster recovery.
During the procedure, the surgeon uses a specially designed proctoscope with a Doppler ultrasound probe to locate the hemorrhoidal artery that supplies blood to the hemorrhoid. Once located, the surgeon ties off the hemorrhoidal artery using a suture, which causes blood flow to the Hemorrhoid to be halted. This leads to the atrophy of internal hemorrhoids, which shrink and either fall off or are absorbed by the body.
Transanal hemorrhoidal artery ligation performed with Doppler-guided guidance is less invasive and painful than other surgical methods. The procedure can be performed under local anesthesia, allowing patients to return home shortly after the procedure.
The benefits of THD for internal hemorrhoid removal surgery are numerous. It is a minimally invasive procedure, minimizing the need for pain medication and hospital stays. Since no cutting is involved, patients can return to normal activities quickly. The success rate is relatively high, with most patients reporting a significant improvement in symptoms post-surgery.
Hemorrhoid Injections

An injection is the standard method for the removal of internal hemorrhoids. An injection of a solution into a hemorrhoid causes it to shrink and fall off. The answer usually has a sclerosing effect on the affected tissue, leading to scarring of the area and cessation of blood flow to the hemorrhoids.
The injection method is typically used for treating minor to medium-sized hemorrhoids that have not prolapsed, meaning they have not protruded from the anus. The procedure is relatively painless and requires no anesthesia, and patients can usually return to their normal activities immediately after treatment.
Using injections to remove hemorrhoids is a safe and easy method. With no incisions or sutures, the risk of complications such as bleeding or infections is minimal.
Patients can also enjoy quicker recovery time compared to traditional surgical methods. For hemorrhoids, the injection method means no discomfort or downtime.
Several studies have demonstrated that injection is a highly effective way to treat hemorrhoids. It provides long-term relief> from symptoms and results in a high success rate.
Moreover, it's a relatively low-cost procedure compared to other surgical methods, making it an appealing option for patients with limited financial resources.
Say goodbye to hemorrhoid pain and discomfort with the injection method.
Surgical Hemorrhoid Removal

Also known as hemorrhoidectomy, Surgical Hemorrhoid Removal is a medical procedure intended to remove internal hemorrhoids that have become enlarged or prolapsed.
If you are a patient who has not seen any improvement through other treatment methods, such as medication or lifestyle changes, this type of surgery is recommended. Say goodbye to the discomfort and inconvenience caused by internal hemorrhoids with this effective solution.
During the procedure, a surgeon will use various techniques to remove the hemorrhoid, including cutting it out, tying it off with a rubber band, or using a laser. In this technique, hemorrhoids are cut off from their blood supply, causing them to shrink and disappear.
A surgical hemorrhoid removal typically takes place under general anesthesia, so the patient will be asleep. Patients can expect to experience some pain and discomfort following the surgery, but this can be managed with pain medication and proper aftercare.
The patient will be asleep during surgery to remove hemorrhoids under general anesthesia. These include bleeding, infection, and damage to the surrounding tissue. Patients should discuss these risks with their surgeon before undergoing the procedure.
The surgical removal of internal hemorrhoids is highly effective in treating swollen and prolapsed hemorrhoids. It's the best treatment option for patients who did not see any improvement from other methods.
By cutting off the blood supply to the hemorrhoid, it can eventually shrink and be removed. Although risks are involved, this technique is highly reliable for treating internal hemorrhoids.
Diagnosis and Treatment Options

Diagnosing internal hemorrhoids involves a physical exam and various tests, such as anoscopy and sigmoidoscopy. Treatment options range from conservative, non-surgical methods, such as lifestyle changes, dietary modifications, and non-prescription medications, to surgical procedures, such as hemorrhoidectomy, stapled hemorrhoidopexy, and sclerotherapy.
Risks and Complications of Internal Hemorrhoids Surgery s

Complications and risks associated with internal hemorrhoid removal surgery may include post-operative pain, bleeding, infections, fecal incontinence, and recurrence of hemorrhoids. Patients should be aware of these risks and discuss them with their surgeon before surgery.
Before undergoing surgery, there are a number of contraindications and factors to consider.
Patients should consider pregnancy, age, overall health, and alternative treatments before undergoing internal hemorrhoid removal. Make a well-informed decision to ensure a successful and safe surgery.
Pregnant women may not be eligible for surgery, depending on the pregnancy's stage and the type of procedure. Age and overall health may also impact eligibility and surgical outcomes.
Alternative treatment options, such as dietary modifications, lifestyle changes, and non-prescription medications, may be recommended before surgery.
When conservative methods fail to reduce hemorrhoids, internal hemorrhoid removal surgery may be a viable option. The recovery process may require several weeks of home care instructions, pain management, hygiene management, and gradual resumption of daily activities and work.
Patients should also be aware of the potential complications and risks associated with surgery and consider various factors before undergoing the procedure.

Recovery Process after Internal Hemorrhoid Surgery
After internal hemorrhoid surgery, recovery may take several weeks, depending on the procedure's complexity. Home care instructions may include dietary modifications, pain management, and hygiene management.
Managing pain and discomfort may involve using prescription medications, sitz baths, and ice packs. Resuming daily activities and work may depend on several factors, such as the type of procedure, the patient's job type and responsibilities, and the surgeon's recommendation.
What to Expect on the Day of Surgery?
Internal hemorrhoid removal surgery can leave you with some apprehension about what to expect. You can expect the following after internal hemorrhoid removal surgery, although specifics will vary depending on your individual case.
Preparation Before the Surgery:

The healthcare provider must give you instructions during the preoperative consultation about internal hemorrhoids. The patient will be required to refrain from consuming food and liquids for several hours before the procedure.
This is to ensure that the digestive system is empty, reducing the risk of complications during the surgery. The surgeon might also prescribe laxatives and enemas to ensure that the rectum is thoroughly cleaned, making it easy for the surgeon to access hemorrhoids.
Different Procedures Performed During Surgery:
Several procedures can be performed during internal hemorrhoid removal surgery. It is important to treat hemorrhoids according to their severity and health status. Below are some of the common procedures performed during the surgery.
Coagulation Therapy:
This therapy uses heat, laser, or infrared light to cause hemorrhoids to shrink. A probe is inserted into the anus to deliver the therapy. This is an outpatient procedure, and the patient will likely return home on the same day. The recovery period for this procedure is shorter compared to other procedures.
Excisional Surgical Hemorrhoidectomy:
This procedure involves cutting off the hemorrhoid tissue using a scalpel or a laser. This procedure is more appropriate for large or prolapsed hemorrhoids.
This procedure requires general anesthesia administered by an anesthesiologist. The patient will stay at the hospital for at least one day after the surgery. Recovery can take up to two weeks.
Other Minor Surgical Interventions, When Necessary:
Other procedures can be performed during surgery, such as stapling or sclerotherapy. The surgeon will discuss these options with the patient during the preoperative consultation.
Wound Care After the Procedure:

After the surgical procedure, the patient may experience some bleeding and discomfort. The healthcare provider will prescribe pain medication to manage the discomfort.
To minimize the risk of wound infection, the patient should use warm water to clean the surgical site after each bowel movement. The patient should also avoid using dry toilet paper and moist wipes instead.
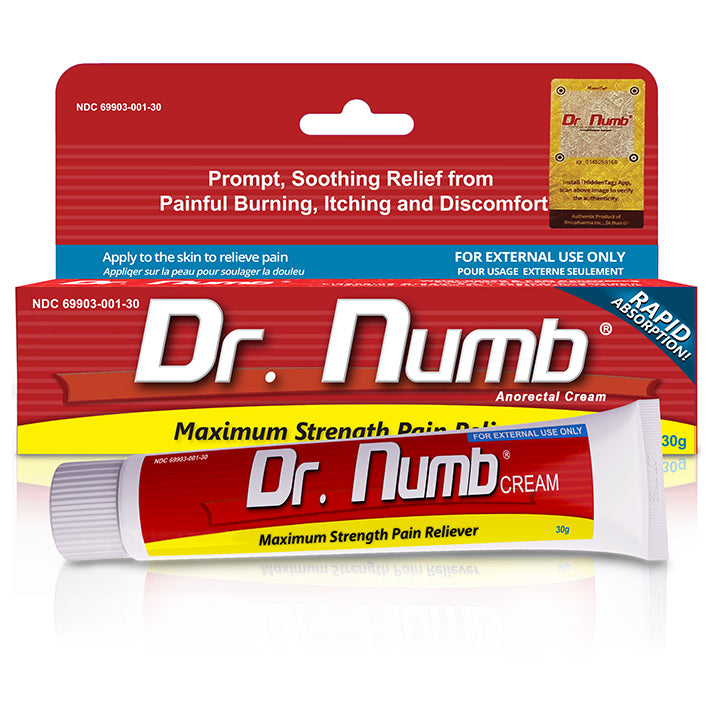
Non-pharmaceutical Treatments for Pain Management and Comfort:
To manage pain and discomfort, the patient can sit on a warm Sitz bath for about 15 minutes several times a day. Using a cushion to sit on will also help reduce pressure on the surgical site.
Physical Activity Restrictions During Recovery
The patient should avoid lifting heavy objects and performing strenuous exercises for at least two weeks after the procedure. This is to avoid pulling the stitches or reopening the surgical wound. The healthcare provider will give more instructions during the postoperative consultation

What to do when you need further assistance. Following the procedure:
The patient should contact a healthcare provider in case of severe pain, excessive bleeding, fever, difficulty urinating, or signs of infection at the surgical site.
Is Internal Hemorrhoid Surgery Painful

Internal hemorrhoids can cause significant discomfort and pain, causing many questions about the potential for painful surgery. There is minimal discomfort with internal hemorrhoids removed by surgery. Local anesthesia or over-the-counter medications like ibuprofen have proven effective in cases of mild discomfort.
Although you may feel some tenderness afterward, surgical alleviation of your condition will ultimately take care of it.
Internal Hemorrhoid Banding Side Effects
Internal hemorrhoid banding is a popular method for treating internal hemorrhoids, but it can still have side effects. A severe case may require medical attention for pain, discomfort, and rectal bleeding.
If you experience any concerning symptoms following the procedure, please get in touch with your doctor immediately contact your doctor.
There have been cases where allergic reactions, urinary retention, or even prolapsed tissue have occurred temporarily during this standard procedure. To make an informed choice, you should discuss all potential risks with your physician before undergoing an internal hemorrhoid banding procedure.
Internal Hemorrhoid Banding Recovery

Recovering from internal hemorrhoids is usually quick and straightforward after minimally invasive surgery. Over-the-counter medications, nutrition, and fluid intake should relieve pain and bleeding during recovery.
For two weeks after the procedure, patients should abstain from heavy lifting and strenuous activities, as well as sexual activity. Healing and discomfort can be relieved by warm baths.
Conclusion
When all other treatments have failed, hemorrhoids are removed surgically as a last resort. Discussing surgical options with a healthcare provider to understand the risks, benefits, and probability of success is important.
The type of surgical procedure performed depends on the size of the hemorrhoid, its location, and its severity. Treatment decisions should consider patient-specific factors such as age, overall health status, and lifestyle choices.
Following the pre and post-operative instructions can hasten the recovery process, prevent complications and avoid unnecessary pain. Healthcare providers should answer patients' questions and clarify any confusion about the surgery.